 CLICK
ON IMAGE
CLICK
ON IMAGE
The basic principle of neurology is to define the anatomy of where the
nervous system is affected and the etiology for what is going wrong.
The anatomy is defined by symptoms, patterns of neurologic loss, and exam
findings. Combinations and patterns of sensory and motor loss help
define many anatomic sites. Without some concept of where the lesion
is, appropriate evaluation with modern imaging techniques cannot be directed.
MRI scans are amazing in revealing abnormalities, but cannot help if you
do not know where to look. The etiology for lesions of the nervous
system relate more to the onset or progression of deficit and often require
confirmation using laboratory screening for specific conditions, e.g. B12
deficiency.
So far in this course you have been exposed to consequences of neurologic
deficits located below the foramen magnum. You should be familiar
with the following anatomic patterns of neurologic loss.
Affects specific muscles, usually proximal muscles giving weakness. No sensory loss.
Myopathies may be inherited and then termed dystrophies. Other
common causes of myopathy are inflammation (polymyositis), endocrine abnormalities
or drugs/toxins.
Neuromuscular Junction
Weakness that is variable and affects some muscles preferentially especially extraocular muscles and oropharyngeal muscles. No sensory loss. Abnormal decremental response to repetitive stimulation.
Sensory and motor findings usually in a glove and stocking distribution.
One system may be more predominant. Lower motor neuron.
Can also have disease of specific nerves either from compression or vascular disease (usually vasculitis or small infarctions associated with diabetes). Common nerves to be compressed are the median at the wrist (carpal tunnel), ulnar at the elbow, peroneal at the fibular head, lateral cutaneous nerve of the thigh at the inguinal ligament. Diabetes often is associated with femoral nerve or other cranial nerve lesions. When multiple nerves are affected the term mononeuropathy multiplex is used.
Pain, sensory, and motor loss. Referable to a dermatome and weakness
in muscles innervated by the same root. Lower motor neuron.
Cauda Equina and Conus Medullaris

Bowel and bladder dysfunction. Sacral sensory loss. May include weakness in S1/L5 muscles. Lower motor neuron.
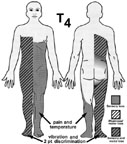
Pushing from outside: hemisection, sacral fibers affected first.
Ipsilateral motor, vibration, two point discrimination, contralateral pain
and temperature. Upper motor neuron.
Pushing from within: sacral sparing, more deficit at the level of lesion.
Upper motor neuron.
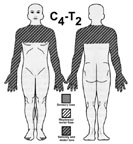
Central cord: bilateral sensory with a cape distribution. Upper
motor neuron. Lower motor neuron at the level of the lesion.
Bowel bladder function may be involved.
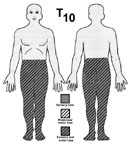
Transverse lesion: bilateral sensory and motor loss with a level corresponding
to the lesion. Bowel and bladder dysfunction.